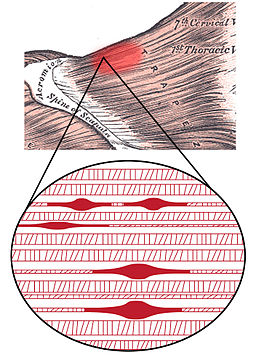
The term trigger point was created in 1942 by Dr. Janet Travell. A Trigger Point Is defined as a hard and hypersensitive nodule or bundle found in a taut band of muscle. Palpating the trigger point will elicit pain in the area and can cause radiation of pain, called referred pain. Trigger Points are often associated with muscle dysfunction, muscle weakness, and a limited range of motion. The reported pain is often out of proportion to the pressure applied. Trigger points often develop in a pre-determined area and will generate a referred pain pattern that is particular to each trigger point.
Trigger Point
The term trigger point and muscle knot are often used interchangeably. However, a muscle knot is not known to cause referred pain or to be specific to a certain area of the body. For that reason, the definitions of muscle knot and trigger point differ slightly. Muscles contract and relax during movement and a muscle knot is formed when a muscle fiber remains contracted, after repetitive use. The causes of trigger points and their association with Myofascial pain syndrome are yet not understood.
There is a debate about the existence of trigger points, with some critical claiming are not the cause of pain, as the specific points can be found in asymptomatic individuals and scientific evidence does not make clear that their disappearance is essential for effective treatment. Nonetheless, In the allied health community, The Manual of Trigger Point and more than 40 articles that Dr.Travell and Dr David Simons wrote still play a fundamental role in defining and popularising the diagnosis and treatment of trigger point. The Manual states that an active trigger point is painful to touch and causes referred pain, and the reproduction of the patient’s symptomatic pain with sustained pressure may confirm the diagnosis of Myofascial pain syndrome.
Many clinicians and patients have felt and experienced tender muscle nodules that referred pain, and have noticed the release and decreased or disappearance of referred pain after having the trigger point treated. The Trigger Point is a common physical finding, but because its cause is also unclear, it is frequently disregarded as a contributing factor to musculoskeletal pain without joint involvement.
There are currently no recognised standards (such as biomarkers, electrodiagnostic tests, imaging, etc.) for diagnosing or characterising trigger point quantitatively, other than the use of palpation. To make the investigation of trigger point and musculoskeletal pain even more complicated, trigger point are common in a wide spectrum of musculoskeletal problems and have been clinically linked to several medical conditions, including those of metabolic, visceral, endocrine, viral, and psychological origin.
The local twitch response is one of the key features of a clinical evaluation that indicates the existence of an active MTrP. An abrupt contraction of the taut band’s muscle fibers is produced by strumming or snapping the band perpendicular to the muscle fibers. Though the cause of the local twitch response is yet unknown, it’s possible that sensitised peripheral mechanical nociceptors are the cause of altered sensory spinal processing.
Travell and Simons’s Trigger Point theory states that abnormal activity within the muscle endplate, an interface between motor neurons and skeletal muscle fibers, results in energy deficiency in the area, which leads to compressed capillaries (compromised blood flow) and increased metabolic demands within the muscle tissue.
Possible Trigger Point Causes and Associations:
- Mechanical stress: Postural (poor ergonometric when sitting or reading); immobility or sustained contraction (holding a power tool/painting); repetitive motion (bruxism); constriction of muscle (bra or belt too tight) or Structural (leg length differences).
- Nutritional Inadequacies – Lack of B1, B6, B12, folic acid, vitamin C, ca, iron, potassium, and magnesium.
- Metabolic and endocrine inadequacies
- Psychological factors – Avoidance of painful movements. Depression (high levels of anxiety can create muscle tension and sustain contraction). Good sports syndrome (stoical attitude, ignoring pain and overloaded muscle). The individual may unconsciously develops psychosomatic symptoms.
- Chronic infections – Viral disease (herpes simplex), bacterial infection and tapeworms or giardiasis (may aggravate trigger points)
- Hay fever (allergic rhinitis) – allergic symptoms must be controlled first.
- Impaired sleep (poor recovery)
- Nerve Impingement (there is a tendency for active trigger points to be present)
Fernández-de-Las-Peñas C, Dommerholt J. International consensus on diagnostic criteria and clinical considerations of myofascial trigger points: a Delphi study. Pain Medicine. 2018 Jan 1;19(1):142-50.
Jay P. Shah, Nikki Thaker, Juliana Heimur, Jacqueline V. Aredo, Siddhartha Sikdar, Lynn H. Gerber. Myofascial Trigger Points Then and Now: A Historical and Scientific Perspective. PM&R 2015, vol 7, p. 746-761.
Simons DG, Travell JG, Simons LS. Travell & Simons’ myofascial pain and dysfunction: upper half of body. Lippincott williams & wilkins; 1999.
Rathbone AT, Grosman-Rimon L, Kumbhare DA. Interrater agreement of manual palpation for identification of myofascial trigger points. The Clinical journal of pain. 2017 Aug 1;33(8):715-29.
Vázquez Delgado E, Cascos-Romero J, Gay Escoda C. Myofascial pain syndrome associated with trigger points: a literature review.(I): Epidemiology, clinical treatment and etiopathogeny. Medicina Oral, Patología Oral y Cirugia Bucal, 2009, vol. 14, num. 10, p. 494-498. 2009 Oct 1.